CAUTION: The following information contains content of a graphic nature to describe the actual methods, dangers, and ramifications of doctor assisted suicide. We do not recommend this lethal practice or advocate for its legalization.
What is Assisted Suicide?
What is Assisted Suicide (AS)? It is Suicide in the practice of individuals obtaining prescriptions (prescribed by doctors or other medical practitioners) of lethal doses of medication to cause their deaths. In states that allow this, a patient must be determined to have a terminal illness defined as incurable and irreversible and will cause death within six months. Proponents say assisted suicide is “medical aid in dying.” They change the verbiage so that legislators will not believe they are voting for assisted suicide.
Where is it legal?
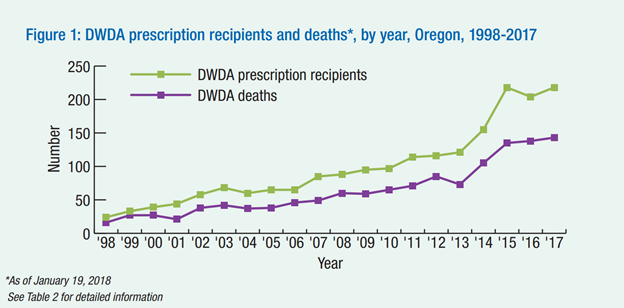
Oregon (first state for over 25 years); Washington State, Colorado, Vermont, California, Hawaii, New Jersey, Maine, New Mexico and Montana (by the Montana Supreme Court) and the District of Columbia.
How is “terminal illness” defined?
Terminal illness or disease means an incurable and irreversible disease/illness that has been medically confirmed and will, within reasonable medical judgment, produce death within six months.
That sounds clear enough, however, the problem is that studies have shown that it is very difficult to accurately predict when death will occur. A patient determined to have a disease that will cause death within six months can live for years.
In a number of states having legal assisted suicide, practitioners are approving patients getting prescriptions who are NOT terminal. The reasons include anorexia, arthritis, arteritis, blood disease, complications from a fall, hernia, sclerosis…and more.
Depression
State laws, like Oregon, require practitioners to refer for consultation if in their opinion, a patient may be suffering from a psychiatric or psychological disorder or depression causing impaired judgment.
If a patient had any one of these, assisted suicide cannot be granted.
However, Oregon studies going back to 1998 found that 25% of patients requesting AS were depressed, but only 3.3% were referred for psychiatric evaluation.
If depression is treated, these patients may not consider AS.
How is it done?
The prescription from a practitioner is given to a patient for pharmacist to fill. The patient can then take the entire prescription at their time of choosing.
Currently, the drug cocktails evolve as patients experience increased times to die. So, these combinations below are experimental:
- DDMP2 is a combination of diazepam, digoxin, morphine sulfate and propranolol.
- DDMA was introduced as a combination of diazepam, digoxin, morphine sulfate, and amitriptyline.
- DDMA-Ph is DDMA above with phenobarbital added.
Death by these combinations does not always happen quickly. Reports have shown patients taking up to 19 hours and more to die. Deaths are not always peaceful or without complications.
WARNING: Immediate death is not guaranteed. Complications include side effects such as nausea, vomiting, seizures and prolonged time from ingestion of the lethal dose until death.[1] Prior to use, take an antiemetic (nausea suppressant) one hour before to prevent vomiting.[2]
Say you are the patient who has requested and received drugs from your doctor to commit suicide.
If you do decide to end your life with the lethal drugs that are now sitting, unattended, in your medicine cabinet. What are they? Death with Dignity explains,
“None of the medical aid-in-dying laws tell your physician exactly what prescription to give you, but all medications under these laws require the attending physician’s prescription. It is up to the physician to determine the prescription.”
Reasons why patients with serious illness choose to think about suicide
Studies by Oregon over years:
- Loss of autonomy (91%)
- Decreased ability to engage in enjoyable activities (90%)
- Loss of dignity (73%)
- Becoming a burden on others (48%)
- Losing control of bodily functions (44%)
- Inadequate pain control or concern about it (27%)
Key problems with oregon and other states’ laws
- Practitioners don’t have to have expertise in the conditions of the patient.
- Second doctor (or practitioner) can be in same office practice as the first doctor.
- Terminal disease definition too broad.
- Practitioner Referral for patient psychiatric evaluation is not often done.
- One of the two witnesses who signs patients’ request can be an heir.
- No requirement that practitioner knows patient for a length of time.
- Allows for doctor/practitioner shopping – if family practitioner refuses to grant request, a patient can find another practitioner to agree, again without knowing the patient.
- Cause of death is to be falsified – death certificate must state cause of death as the underlying cause NOT the suicide.
- Study shows that about 82.4% of 714 practicing U.S. doctors view the significantly disabled as having a worse “quality of life” than nondisabled people.
- There is broad criminal and civil liability immunity for prescribers.
- A patient can be alone when taking the drugs – no practitioner or family need be prsent even though serious complications to the patient can occur.
- Death does not always come fast – it could be hours or even a day before death occurs.
Insurance companies have been known to refuse coverage for the more expensive lifesaving treatments but cover the cheaper drugs for assisted suicide:
- Barbara Wagner: Denied payment for chemotherapy and offered payment for lethal drugs by the State of Oregon. (https.//www.youtube.com/watch?v=2rrNVesLuFg)
- Randy Stroup: Denied payment for chemotherapy and offered payment for lethal drugs by the State of Oregon. (https.//www.youtube.com/watch?v=fKOT3oujULI)
- Stephanie Packer: Denied payment for lifesaving treatment and, when asked, was told by her California insurance company that they would pay for lethal drugs for only a $1.20 co-pay. (https.//www.facebook.com/cbcnetwork/videos/10154641061607079/)
- Patients of Dr. Brian Callister: Denied payment for lifesaving treatments and offered payment for lethal drugs by insurance companies in Oregon and California, even though the patients had not requested them. (https.//www.youtube.com/watch?v=CWrpr_5e4RY)
- Canadian officials estimated that assisted suicide and euthanasia could reduce annual spending by between $34.7 and $138.38 million compared to $1.5 million spent on lethal drugs. (3 Aaron J. Trachtenberg, MD DPHil; Braden Manns; MD MSc, “Cost Analysis of Medical Assistance in Dying in Canada, CMAJ 2017 Jan 23; 189(3); E101-E105. https//www.ncbi.nim.nih.gov/pmc/articles/PMC5250515/)
Disability Rights Concerns:
The disabled see biases against those with disabilities
Help for the disability community to remove consideration of assisted suicide would best happen if there were more wrap around services including but not limited to:
- Legislation to provide support in transitioning out of nursing homes
- Medicaid waivers to cover community housing
- Legislation to provide better aid in transportation
- Legislation to provide better aid in jobs
- Legislation to provide a larger monthly personal needs allowance
Assisted suicide laws:
You may have been told that a bill to legalize assisted suicide has strict requirements that must be met before someone can receive drugs to end their lives – this is misinformation! The reality is that the “strict” requirements are not as strict as they seem, and often when a bill becomes law, the safeguards originally in place are later removed because they are viewed as barriers to those who wish to see it explained.
The Problem of Terminal Illness – you may have heard that states with assisted suicide laws only allow assisted suicide for the “terminally ill” patient with six months or less to live and with the approval of two doctors. The definition of “terminal illness” is arbitrary and includes patients who are not dying. For example, if a patient refuses to take his/her heart medication, that patient is then defined as “terminally ill” and eligible for life ending medications. How many times have you heard of someone who has been given a terminal diagnosis and they live well beyond the time a doctor thought they had?
Additionally, a number of states that have “assisted suicide” laws are not including non-terminal reasons for approving “assisted suicide” such as anorexia nervosa, arthritis, diabetes, and other non-terminal diseases.
The Problem of Doctor Shopping: Often, a patient’s personal doctor, who has long known the patient, refuses to sign an order for medication for assisted suicide, and then the patient doctor shops. Most doctors will not approve of suicide so proponents will simply take cases to the small percentage of doctors they know will approve it for anyone seeking to end their life.
The Problem of Expertise (or the lack thereof) – Similar laws do not require that the doctors who sign the order have to have expertise in the particular diseases or conditions that the patient has who is seeking assisted suicide. A doctor with the right expertise may have more options to help the patient get treatment than a general practitioner.
The Problem of Mental Health – Assisted Suicide laws in other states generally require that if a patient has mental health problems, like depression or a psychosis, they cannot be allowed to obtain assisted suicide medications. However, in a study from Oregon, the state that has had an assisted suicide law for 25 years, found that even though its own law requires the doctor to refer a patient that shows signs of depression or a mental problem for a psychiatric evaluation, only 3.3% of patients were referred for evaluation according to reports going back to 1998.
The Problem of Supervision – After the patient is prescribed the lethal drugs, there is no legally required supervision of the patient in taking the drugs. A patient can be and frequently is alone when he/she takes the drugs. Additionally, death does not always come fast – it could be hors or even a day before death occurs with those patients suffering for hours.
Assisted suicide increases suicides in general
- When assisted suicide becomes socially acceptable through legalization, suicides in general increase.
- The National Council on Disability report notes that before Oregon legalized assisted suicide, its suicide rate was similar to the national average. However, by 2010, Oregon’s suicide rate was 41% above the national average.
- Further, a 2015 article in the Southern Medical Journal found that states with assisted suicide laws are associated, on average, with a 6.3% increase in total suicides. For individuals older than 65, the increase was 14.5%.
- An op-ed published in the The Washington Post a month later by Aaron Kheriaty, associate professor of psychiatry and director of the medical ethics program at the University of California Irvine School of Medicine, noted the unsurprising results of the study.
“You don’t discourage suicide by assisting suicide…publicized cases of suicide often produce clusters of copycat cases, often disproportionately affecting young people, who frequently use the same method as the original case.”
- This comes at a time when the suicide rate in the United States increased 33% from 1999 through 2017, according to the Centers for Disease Control and Prevention. Since 2008, suicide has ranked as the 10th leading cause of death for all ages. Suicide also ranked as the second-leading cause of death for ages 10-24 in 2017, the most recent year for which data are available. Shockingly, the suicide rate among those aged 10-24 increased 56 percent from 2007 and 2017.
In 2021, the Illinois General Assembly passed HG 1778, with virtually no opposition, which provides that “each school district that serves pupils in any of grades 6 through 12 and that issues an identification card to pupils in any grades 6 through 12 shall provide contact information for the National Suicide Prevention Lifeline, the Crisis Text Line, and either the Safe2Help Illinois helpline or a local suicide prevention hotline or both on the identification card.” For public higher education institutions, the same must be done on the students’ cards.
This was in addition to at least five statutes that many lawmakers voted for to support mental health and suicide prevention efforts for all persons, including a large list of persons who might be most vulnerable.
This includes:
- 105 ILCS the School Code – Sec. 2-3.166 Youth Suicide Awareness and Prevention
- 410 ILCS Department of Public Health – Sec. 5. “In 2004, the Illinois General Assembly passed the Suicide Prevention, education, and Treatment Act…to establish the Illinois Suicide Prevention Strategic Planning Committee to develop the Illinois Suicide Prevention Strategic Plan.”
- 110 ILCS Higher Education – Sec. 65-5 The General Assembly finds that “There are insufficient behavioral health professionals in this State’s behavioral health workforce and further that there are insufficient behavioral health professionals trained in evidence-based practices.”
- 405 ILCS Mental Health and Developmental Disabilities – Sec. 7-1 Community-based pilot program for the “development and implementation of a comprehensive and coordinated continuum of community-based pilot programs for persons with or at risk for a mental health diagnosis that is sensitive to the needs of local communities.”
- 50 ILCS Local Government – Sec. 10.24 Officer wellness and suicide prevention.
- And other statutes.
A proposed assisted suicide bill (under a phony name like “Medical Aid in Dying”) will undermine all these efforts to support Illinoisans who are suffering under mental health problems and who need our support to get well and receive treatment.
Allowing Assisted Suicide Laws into illinois enables deadly dangers towards people with disabilities
Not one single major national disability rights organization supports assisted suicide laws and all with positions, oppose them. This includes The National Council on Disability, a presidentially appointed, federal agency that has advised every administration since the Clinton administration to strenuously oppose assisted suicide laws which puts the most vulnerable in society at risk of deadly harm and which are inherently dangerous. The breadth and depth of the dangers can be read in part below:
- Doctors who are to decide which patients qualify under the requirements of the law do not have to know the patient for more than 15 days and do not have to have expertise or specialty in the field of the patient’s illness or disease. If the patient’s long time personal doctor refuses to prescribe the lethal dose, the patient can just find another doctor who will. This practice is called doctor shopping.
- The doctor is not required to be present when the patient “ingests” the lethal, prescribed medicines. Reports have shown that only about 23% of “assisted suicide” patients have a doctor present. (Physician-Assisted Suicide in Oregon – A Medical Perspective – Michigan Law Review – Vol. 106:1613)
- It is only required that the doctor, in his/her opinion, refer the patient for consulting if the doctor thinks the patient may be suffering from a psychiatric or psychological disorder or depression causing impaired judgment. Reports from the Oregon Public Health Division have shown that “the percentage of cases referred for psychiatric evaluation dropped from thirteen percent between 1998 and 2005 to four percent in 2006.” “The wish for death is a ‘cry for help,’ a reliable sign of depression.” Researchers have found hopelessness, which is strongly correlated with depression, to be the factor that most significantly predicts the wish for death.”
The disabled are in danger under “Assisted Suicide” laws:
- “Although people with disabilities aren’t usually terminally ill, the terminally ill are almost always disabled since terminal illnesses are almost always disabling in some way, particularly in the latter stages.” (NotDeadYet.org – Why We Oppose Assisted Suicide Laws)
- Depression and major depressive disorder are DISABILITIES according to the Americans with Disabilities Act.
- Described in 2006 by H. Rex Greene, M.D. “the psychosomatic literature describes… Demoralization Syndrome, which is very common in chronic…life threatening illness, the features of which (hopelessness, helplessness, and despair) fit the profile of the victims of Oregon’s law, who are consistently reported NOT to be in pain or disabled by their allegedly terminal illness but request (assisted suicide) because of fears of what might come in the future: helplessness, dependency, becoming a burden.” (Disability Rights Education & Defense Fund DREDF – Fear, Bias, and Prejudice Against Disability)
- There’s an established body of research demonstrating that physicians underrate the quality of life of people with disabilities compared with our (disabled) own assessments.
- Assisted Suicide laws set up two different approaches to the medical model for caring for patients with medical and mental health condition: (Physician-Assisted Suicide in Oregon – A Medical Perspective – Michigan law Review – Vol. 106:1613)
- The medical model in the states is for patients requesting assistance in suicide to be assessed in the same way as other patients intent on suicide. The medical model recognizes that “although physical illness may be a precipitating cause of despair, these patients usually suffer from treatable depression and are (almost) always ambivalent about their desire for death. Study of terminally ill cancer patients has demonstrated that those preoccupied with assisted suicide had symptoms of depression or hopelessness.”
- The Oregon assisted suicide model (along with other states with assisted suicide) take “a totally different approach. It stresses that any mental health consultation should be an evaluation of competency focused on the patient’s capacity to make a decision.”
- “Whether or not one agrees with the majority of clinical psychiatrists and forensic psychiatrists, who believe that the presence of major depressive disorder should result in an automatic finding of incompetence’ to make decisions about assisted suicide, reducing the psychiatric consultation to the issue of competency ignores all the other psychological factors that go into the request for assisted suicide.”
- “Arguments for Assisted Suicide are not about terminal illness, but “indignity” in needing help to eat, move, breathe, or take medications.” (Article in DREDF in Section D. Disability – Aid in Living, not dying) “The answer of (of a health care system that is failing people with disabilities), however, is to make sure that people with illness-related disabilities are receiving the supports and services they need in order to live – not to create a new fast track toward death.”
Watch, listen, and learn.
A practicing physician in the state of Oregon, Dr. Charles Bentz has experienced the legalization of doctor assisted suicide (DAS), first-hand. Having cared for patients nearing the end of life or suffering from terminal conditions, he’s received requests from patients for physician assisted suicide. Sharing his knowledge and personal experience with PAS, we will come to understand the reality and ramifications of this practice.